In my post about the pregnancy and prenatal care options I chose, I mention that I don’t take the pregnancy glucose test that requires drinking glucola (that syrupy orange or grape drink) and that I use an alternate method of testing. I’ve gotten so many questions about this that I decided it deserved its own post, especially while I am still pregnant and the topic is fresh on my mind.
IMPORTANT: Please note that I am only writing about my own personal experience with this and the decisions I made after consulting with my OB or midwife (depending on which pregnancy it was). The information in this post (or any post I write) is not medical advice in any way… I’m just sharing my experience. Always consult with your own medical providers before making health decisions, especially during pregnancy, and make sure that you find providers who are willing to work with you to make the best decision for your pregnancy.
All that being said, here’s what I do when it comes to the pregnancy glucose test.
What is the Pregnancy Glucose Test?
This was one of the sections I found in all of the many pregnancy books I read when pregnant with my first child. Current guidelines call for a glucose challenge test somewhere between 24-28 weeks of pregnancy to test for gestational diabetes.
This test typically involves drinking a sweetened drink called Glucola that contains 50, 75, or 100 grams of sugar in different forms. In most cases, the first part of this test is an Oral Glucose Challenge Test (OGCT) that involves drinking the 50 gram solution and having a blood test exactly one hour later to measure blood sugar. If a woman passes this test, she typically won’t be given further testing for gestational diabetes. If a woman does not pass the test, a longer test involving a higher level of glucose consumption may be used.
It is important to note that for this test, it is the amount of glucose present, not the drink itself that is important for measuring blood sugar levels.
Why Test for Gestational Diabetes?
This was one of my original questions and one that I researched in depth. I didn’t have a personal history of diabetes or even a strong family history of it, so I wondered if the test was even necessary. I found that rates of gestational diabetes (a type of glucose intolerance that occurs during pregnancy that often resolves itself once the baby arrives) had risen dramatically in recent decades.
Gestational diabetes (GD) has its fair share of risks and is very important to be aware of and proactive about if a pregnant mom has it. Estimates suggest that 5-10% of pregnant women in the US may have some level of gestational diabetes and since it can increase rates of many pregnancy and birth complications, it is important to correctly identify these women. At the same time, it is important to note that a woman’s body does naturally become slightly more glucose intolerant during pregnancy as the baby needs a steady supply (though not a large supply) of glucose for development.
Managing Gestational Diabetes
Gestational diabetes can often be regulated by diet, though insulin is sometimes needed. Untreated GD can lead to serious complications like increased rate of c-section & shoulder dystocia, babies larger than they should be for their gestational age, higher rates of preeclampsia in mom and low blood sugar in baby at birth.
Certainly, gestational diabetes is a serious problem and one that I absolutely wanted to rule out in my pregnancies, I just wondered if there was a more effective way to test for it.
My Concerns with Glucola
While I agree that it is important to test for gestational diabetes, I had concerns with the glucola test itself, mainly that it contained ingredients I would not normally consume while pregnant (or ever!) and that it has a higher amount of sugar than I would consume at any one time. Most women describe this drink as tasting like an un-carbonated and syrupy orange soda. No thanks!
Glucola Ingredients
The ingredients in the pregnancy glucose test vary depending on the specific type of glucose drink consumed, but most that I was able to find a label for contain food dyes, brominated vegetable oil (BVO), dextrose from corn, and other substances that I consciously avoid.
At the very least, I was annoyed about the presence of food dyes (which give me a headache) as they are not needed for the effectiveness of the test and are merely there to make the drink look better (and hint: it doesn’t make it taste better at all!). Some women have allergies to corn and citric acid, so the glucola test is not even an option for them anyway.
What is BVO?
The added dyes and BVO are not needed for the effectiveness of the test as there must be a specific amount of sugar and blood tested at a specific time. With my first pregnancy, there was not a dye-free and BVO-free option, although there now is (it is not commonly used yet though).
I was surprised to find that BVO (and many food dyes) are banned in other countries but still consumed here. At a time when I am extremely careful about consuming only whole, natural foods, it seemed counter-intuitive to drink something with such controversial ingredients.
I’m also well-aware of the common objections that women get when they question the ingredients in the Glucola- mainly that a woman should “be no more concerned about this than a can of soda during pregnancy” (which I don’t drink) or any other sugary or dye-containing food (which I don’t eat). Yes, at the end of the day, it is not likely that a mom or baby will have a life-threatening or even life-altering reaction to the Glucola drink, but this test may not be the most effective option either (and certainly not the most pleasant).
The Sugar Content
I also would not consume 50 grams (and certainly not 100 grams!) of processed sugar at any point during pregnancy and certainly not by itself. The test required fasting from midnight the night before the test and drinking minimal water during that time. Then, drinking what would essentially be almost my entire carbohydrate intake for an entire day in one sitting in processed form.
I questioned if this was actually a reliable way to test at all, since my body wasn’t normally dealing with these amounts of sugar. I realize that many people do consume this amount of sugar (and food dyes and dextrose) on a regular basis, but for me personally this test was not an accurate representation of the amount of sugar my body would have to handle normally.
Also, if the 50 grams of sugar was the important part of the test, why did it have to come from an artificially flavored and colored source? Couldn’t it come from another food or drink as long as it contained the same amount? Some research showed that not only was this possible, but it had already been studied. This study showed no difference in outcomes when subjects consumed 28 jelly beans instead of the glucose drink.
Bottom Line About the Glucose Drink & Test
It contains unnecessary additives for color/taste that, while not well studied in the US, have been banned in other countries. In the grand scheme of things, consuming a small amount of these ingredients in a single dose during a glucose test is probably not going to cause long-term health problems and may just result in a mom not feeling well for several hours.
Undiagnosed gestational diabetes is a potentially much bigger problem than the additives in the drink, but considering the additives are unnecessary for the effectiveness of the test, I hope that the medical community will continue to research these ingredients and develop a dye and BVO-free version.
Is the Glucose Challenge Screening Accurate?
I also had questions about the accuracy of the glucose challenge screening for the following reasons:
False Positives
There is a high rate of false positives on the 1-hour glucose challenge test. In fact 15-20% of women will test positive on this test, but only 2-5% of women will test positive on the follow-up test or be diagnosed with gestational diabetes (though a positive on the 1-hour test can be a risk factor it itself). There seems to be a higher rate of this if mom does not normally consume sugar in these amounts.
Additionally, since pregnant women are not advised to fast or restrict water at any other point of pregnancy, this may be part of the problem as the test is often done after a long period of fasting. It is also important to remember that the OGCT is simply a screening test and not a true diagnostic test. A study found sensitivity and specificity of the 1-hour glucose challenge test were 27% and 89%, respectively, with a prevalence rate of 5%.
Could the test be wrong?
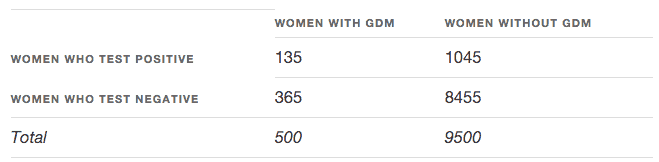
In fact, as “The Pregnant Mathematician” points out, when the test is evaluated mathematically, there is both a high rate of false positives and false negatives in women who may actually have GD. She breaks down the math:
Let’s assume we give the same 1-hour glucose challenge test to 10,000 pregnant women. With a prevalence rate of 5%, we would expect 500 women to have GDM and 9500 not to have GDM. Of the 500 with GDM, since the sensitivity is 27%, we know 27% of 500 would screen positive, for a total of 135 women. These are women who have GDM and whose screening will come back positive. Meanwhile, of the 9500 women without GDM, since the specificity is 89%, we would expect 89% of 9500 or 8455 women to have a true negative result.
According to this table, a total of 135+1045=1180 women would test positive. Of the women who get a positive result, only 135 of them really have GDM; this is the positive predictive value and, in this case, it’s 135/1180 = 11.44%.
Of the women who test negative- Out of 8820 only 8455 would actually not have GD. This gives a negative predictive value of 8455/8820 = 95.86%.
What does that all mean? If you aren’t into the math, it means that there is a decent chance that a woman who doesn’t have GD will receive a false positive and also a chance that a woman may test negative and actually have GD.
Differences Depending on When Test is Taken
Another study showed that results varied noticeably depending on when the glucose challenge test was given. Since glucose rises naturally as pregnancy advances, it is possible for a women to pass the OGCT if taken earlier (23-25 weeks) but fail if taken later in pregnancy (28-30 weeks).
Screening, Not Diagnostic
As this is just a screening test with room for error that is testing for a problem with the potential for big complications, I decided to find out if there was a more accurate alternative that could be used instead of or in addition to the 1-hour glucose challenge test.
Are There More Effective Alternatives?
Food and Drink Alternatives to Glucola
As I mentioned, there are dye-free and BVO-free alternatives to the drink, though they can be difficult to find and it seems that many doctors are not aware of them.
Some doctors provide alternatives to glucola and I have friends who (at the advice of their doctor) instead consumed things like:
- 6 ounces organic grape juice + a banana
- 1 cup milk + 1.5 cups cereal
- Pancakes with 1/4 cup maple syrup
- 28 dye-free jelly beans
- Natural soda with 50 grams total sugar
- 16-ounces orange juice
These options are not as well-studied as the glucose drink but are often much more palatable to a pregnant mom. It is important to note that these options are not straight glucose but contain a mixture of glucose and fructose (and other starches/sugars).
Even if effective, these options will also have the same statistical problems as glucola for the screening test and may miss women who have GD or falsely identify women as positive who actually do not have GD.
Blood Sugar Monitoring
After much researching and talking to my doctor and midwives, I eventually chose what I found to be a more effective and accurate way to test my blood sugar: blood sugar monitoring.
In fact, this is considered so effective that it is part of a regular monitoring program for people who have diabetes and women who are diagnosed with gestational diabetes are often required to monitor their blood glucose anyway.
At-home glucose monitoring is also used to help identify if a woman has GD after receiving a positive on the OGCT, so I skipped the screening and went straight to the diagnostic/monitoring with blood glucose testing.
Sure, the finger stick isn’t fun (though I’d argue it is more fun than drinking syrup), but it provides a much more accurate look at the body’s response to glucose on a daily basis. Additionally, this option can be easily done at home and once I received the “ok” from my doctor/midwives, I was able to get the supplies for at-home monitoring for less than the price of the OGCT with our insurance.
Here’s Why I Chose Blood Sugar Monitoring
It provided a more long-term view of what my glucose levels were doing and more insight into how individual foods affected by blood sugar on a daily basis. Additionally, it let me monitor throughout pregnancy, not just in a one-hour window at 28 weeks, and adjust my diet based on my personal readings.
In fact, after talking with my doctor, this is an option I would personally choose in addition to taking the 1-hour glucose challenge test if I was going to take it. Given the high rate of false positives and negatives on the OGCT, actually monitoring blood sugar is a more accurate way to keep an eye on blood glucose levels throughout pregnancy.
Many women who do have GD are able to manage their condition with diet alone under the guidance of a doctor and nutritionist by consuming whole foods and reducing processed carbohydrate intake. I already consume a real-food diet and limit all processed foods, so I found that monitoring my blood sugar at home was a fascinating glance into how my body handled different foods.
In fact, I was surprised to find that white rice didn’t affect my blood sugar as much as I expected, but certain fruits did.
For glucose monitoring, I use Levels and highly recommend them. They make continuous glucose monitoring mainstream for the first time ever and the data is fascinating! In addition to providing you with CGM sensors, the Levels app interprets your data, scores your individual meals, and allows you to run experiments across different inputs like diet, exercise, and allows you to see your glucose levels with one touch of your phone.
What I Did
At around the 28-week mark of pregnancy, I always tested my blood sugar for about a week at the following times:
- Fasting reading as soon as I woke up
- 1-hour after each meal
- 2-hours after each meal if reading was not below 120 at 1-hour
- Several times after purposefully consuming a really high-carb meal
- At other times just out of curiosity, including a few times after purposefully eating about 50g sugar just to see how I would have done on the OGCT
At my doctors recommendation, these were the ranges I was looking for to make sure my blood glucose was in a healthy range:
- Fasting blood glucose (first thing in the morning) of 86 or lower (Mine ranged from 81-85)
- 1 hour after eating= 140 or lower (mine was always below 120)
- 2 hours after eating= 120 or lower (mine was usually around 100)
- 3 hours after eating= back to fasting level (yep)
There can be some variation in this, but the majority of my readings should be in these ranges. I do this at 28 weeks and 33 weeks (my preference) and also throughout the last trimester to make sure my levels are good.
Hemoglobin A1C Test
I should also note that in regular blood testing and monitoring with my doctor for my thyroid during this pregnancy, I also had my Hemoglobin A1C tested at several points. This test is run as part of the regular panel at my local lab and it is also a test used in monitoring and controlling diabetes as it measures average blood glucose over a period of 3-months. It has been used as an alternative to oral glucose testing in some patients and is routinely used for patients with regular (non gestational) diabetes. I didn’t specifically use this test as an alternative to other forms of GD testing but considered it good insurance since my levels were well within normal.
Bottom Line: My Hope for The Future of GD Testing
I share this information just as a mom who has been through it six times and not as a medical professional of any kind. Any pregnant woman should absolutely work with her doctor or midwife to determine the safest and most effective form of testing for her and her baby.
My hope is that as more women question the need for unnecessary ingredients in the glucose drink, dye and preservative free options will become more common and easy to find. Yes, the levels of dyes and preservatives in current options are pretty low, especially if it is only consumed one time, but this drink is routinely given to all pregnant women and there is absolutely no medical reason for the additives and no reason to expose unborn babies to them, no matter how small the risk!
Improved Accuracy?
There are also some concerns with the rates of false positives and negatives with the 1-hour oral screening test, and it is simply that: a screening test and not a diagnostic one. As I said, I don’t think that women should refuse the test and do nothing, but I have my doubts about the accuracy of the test and think that there are potentially much better options to a one-hour glance of blood glucose at 28-weeks.
I hope that more women will question the presence of these additives in the glucose drink and take a more active role in working with their healthcare providers to decide if the current OGCT is the best option for them. Many doctors and midwives seem to be open to alternative testing measures like dye-free glucola and at-home blood sugar monitoring.
What I did:
My personal choice, after consulting with my own health practitioners, is to focus on a very nutrient-dense whole-food diet that contains enough protein, healthy fats and vegetables throughout my pregnancy (which is similar to the diet recommended for a woman with gestational diabetes anyway) and to test my blood glucose at home throughout pregnancy as a more accurate way of accessing my risk of GD.
I didn’t “refuse” the OGCT (as I wasn’t asked to take it) but chose a more involved method of testing and monitoring that I felt provided a more accurate picture of blood glucose levels and actual risk of gestational diabetes. (And my results were normal with all of my pregnancies and my babies ranged in weight from 6.5 to 7.5 pounds).
Did you drink the glucola? What were your results?
Interested in a more natural pregnancy?
Sign up for the world’s first pregnancy week-to-week series from a *natural* perspective! Created by my friend Genevieve from Mama Natural, the series shows you what’s up with baby, mama, and more each week. You’ll discover natural remedies for various pregnancy symptoms and prepare for your best and most natural birth!
Click the image below to get access now!



Leave a Reply