While I’ve primarily dedicated this website to the everyday experience of being a mama, not everyone wants a large family. Some women feel their family is complete and it’s not in their plan to become pregnant again (or at all). Here are the non-hormonal birth control options I’ve used in my own family planning.
Birth control is common these days for a variety of reasons. According to the CDC, almost 25% of women aged 15 to 49 currently use a hormonal contraceptive. These include “the pill,” a diaphragm, or intrauterine devices (IUDs).
So it’s no surprise that I’ve gotten dozens of requests for natural birth control options. Women are constantly asking for natural alternatives to hormonal contraceptives. As an introvert, I tend to shy away from controversy. Still, I decided to tackle this head-on.
How Do Hormonal Contraceptives Work?
I have a plethora of non-medical reasons for avoiding hormonal contraceptives. But there are some solid medical/scientific reasons to make this decision, too. Hormonal contraceptives are artificial hormone-like substances that mimic the effects of naturally-occurring hormones. According to the FDA, these contraceptives work by:
- Interfering with ovulation. Estrogen and progestin in the pills stop the ovaries from releasing eggs.
- Thickening the cervical mucus, which prevents sperm from reaching the egg in the fallopian tube.
- Disrupting the ability of the fallopian tubes to move fertilized eggs from the ovaries toward the uterus.
- Preventing the buildup of the uterine lining which, inhibits implantation of a fertilized egg.
For me, the possibility that you could conceive but the fertilized egg wouldn’t implant is disturbing. It’s enough to keep me from ever wanting to use hormonal contraceptives. And there’s a long list of other reasons. But it turns out artificial hormones also damage women’s health.
(They also damage environmental health when they end up in the water supply).
Why Avoid Hormonal Contraceptives?
There are plenty of health reasons to avoid hormonal methods of birth control. Hormonal contraceptives impact way more than your hormones. Using them can undermine your health over time or even lead to new health conditions.
May Cause Nutrient Depletion
Many medications affect how we absorb nutrients, which can cause deficiencies. Hormonal contraceptives are no different. Researchers have found these medications deplete key vitamins and minerals. This can be detrimental to reproductive health, bone health, the brain, the immune system, and more.
A 2011 randomized controlled trial found hormonal contraceptives deplete certain nutrients. This includes vitamin B6, zinc, selenium, phosphorus, and magnesium. These deficiencies can lead to other health problems thanks to the important role these nutrients play.
Vitamin B6 and magnesium are critical for hormone balance. The minerals zinc and selenium are crucial for the immune response. Phosphorus makes strong bones.
Another hormonal birth control method is a transdermal patch. This method delivers synthetic estradiol directly into the bloodstream. It may cause significantly lower levels of coenzyme Q10 and alpha-tocopherol. When the body is low in these nutrients, it can lead to increased oxidative stress, inflammation, and calcification.
Besides depleting these nutrients, the pill can also lead to an excess of copper, calcium, and iron. This can then exacerbate deficiencies in other nutrients.
May Cause Depression or Anxiety
Depending on the type of pill and its ingredients, hormonal contraceptives can cause or worsen depression or anxiety. This seems to occur more often in those with a personal history of mood disorders or a family history of mood disorders.
May Lead to Low Libido, Sexual Dysfunction, and Infertility
While women often take hormonal contraceptives to help them enjoy sex risk-free, it doesn’t always turn out that way. The use of these pills may compromise your sexual health. A 2001 study in Human Reproduction found hormonal birth control may decrease your interest in sex.
A 2014 study reports it may also cause issues down there that decrease pleasure. Plus, if you decide you want to have a baby down the road, it may be more difficult.
May Cause Blood Clots
Blood clots are a significant risk of certain pills. While blood clots from taking the pill are rare, they’re a big deal because they can be fatal. Yaz and Yasmin in particular have been linked to blood clots. According to a 2011 warning by Health Canada, a woman using Yaz has a 1-½ to 3 times increased risk of blood clots compared to other birth control pills.
May Contribute to Cardiovascular Disease
Women who use low-dose oral contraceptives have double the risk of a fatal heart attack compared to those who don’t. A 1990 review found ladies who use oral contraceptives and smoke have 12 times the risk of fatal heart attacks. Their rate of fatal brain hemorrhages is three times higher.
The British Journal of Obstetrics and Gynaecology conducted a clinical trial of women with a history of migraines. They found that those who take combined oral contraceptives have 2-4 times the risk of stroke compared to those who don’t take the pill.
May Lead to Blood Sugar Issues
A 2003 journal article found oral contraceptives may aggravate insulin resistance. This is because they decrease insulin sensitivity and glucose tolerance. As a result, these medications may increase your long-term risk of diabetes and heart disease.
May Increase Your Risk of Cancer
A study by the World Health Organization tied contraceptive use to cervical cancer. Women who have HPV and have taken the pill for five to nine years have a higher cervical cancer risk. They’re nearly three times more likely than non-pill users to develop cervical cancer.
HPV affects a third of all women in their twenties. And women with HPV who have taken the pill for more than ten years are four times more likely than non-users to develop the disease.
Scandinavian researchers looked at women who use the pill after age 45. They found this age group has a 144% greater risk of developing breast cancer than women who have never used the pill. That’s 144 percent!
With all these potential problems, are hormonal contraceptives worth it? Is it worth risking cancer to regulate your cycles and improve the look of your skin? Thankfully there are much better options!
Taking The Pill For Balanced Skin and Hormones?
Many women use hormonal contraceptives to help “balance hormones,” or “regulate their cycle.” They may even use them just to prevent acne. The problem is that this treats the symptoms but doesn’t address the root cause. The body naturally moves toward balance, so if hormones are out of whack, it’s not from a contraceptive deficiency. It’s that the body isn’t producing optimal levels of natural hormones.
Treating some symptoms of hormonal imbalance with these medications fails to fix the root of the problem. It can also lead to more significant health issues in the future. The underlying imbalance can still cause other problems in the body.
I used to have horrible acne problems! Clean eating and the oil cleansing method really helped clear up my skin. If hormone balance is the goal, check out this article to learn many ways to balance hormones naturally.
Supplements For Hormone Balance
I’ve also found some supplements that help a lot.
- Maca – This hormone-balancing root has a long history of use in Peru. It can help with fertility, reduction in PMS, and better skin and hair. It can also boost male fertility. Maca is a good source of minerals and essential fatty acids so I like using it in smoothies or coffee. You shouldn’t take it during pregnancy though.
- Magnesium – This mineral is vital for hundreds of functions within the human body. Most of us are deficient, but there are several different ways to get magnesium. I like this magnesium powder, especially for staying regular. Ionic liquid magnesium or magnesium oil are both really good.
- Vitamin D – A pre-hormone that supports hormone function. It’s best to get it from the sun if possible, or you can take a D3 supplement. Ideally, get your serum Vitamin D levels checked to track your levels.
- Gelatin or Collagen – A great source of minerals and necessary amino acids. These powders support hormone production and digestive health in various ways. Gelatin powder can actually “gel.” It works well in recipes like homemade jello and probiotic marshmallows. Collagen powder doesn’t gel but easily stirs into soups, smoothies, coffee, tea, or any other food.
- Natural Progesterone Cream – Menstrual troubles are often due to hormone imbalances, like low progesterone. Progesterone cream is especially helpful for those with short cycles. It can also help if you have a short second phase of your cycle (ovulation through the start of menses). If you do use progesterone cream, do your research. Opt for soy-free and only use it during ovulation through menses. Check with a doctor or healthcare provider before using any hormone supplement.
Which Birth Control Methods I Don’t Recommend
There are some non-hormonal birth control methods I don’t recommend. This is due to their potential toxicity, effect on the body, or potential for miscarriage.
Birth Control Sponge
The contraceptive sponge is non-hormonal but it has chemicals. It’s made of polyurethane — a squishy plastic. Then it’s doused with a chemical called Nonoxynol-9. This chemical can irritate your vagina, increasing your risk of infection. Nonoxynol-9 is considered safe for use in personal care products in the United States. But for some reason, the European Union has banned them…
Copper IUD
Gynecologists often recommend copper IUDs as a natural type of birth control. While they’re technically non-hormonal, copper has a major effect on hormones. Copper, when it gets out of balance with zinc, can cause all kinds of health problems. Some of these include estrogen dominance, PCOS, and breast cancer.
Tubal Ligation or Vasectomy
Tubal ligation and vasectomies are both forms of sterilization. They’re 99% effective but can come with risks.
Women often refer to tubal ligations as “getting your tubes tied.” Tubal ligation is a surgical procedure that blocks or removes a part of your fallopian tubes. It prevents eggs from your ovaries from meeting up with sperm in the fallopian tubes. That’s where they would otherwise be fertilized and implant themselves in the uterus.
A vasectomy is also a surgical procedure of blocking or removing tubes. In this case, the small tubes in a man’s scrotum are blocked or removed. The result is sperm cannot leave the body and cause a pregnancy.
Vasectomies can increase the risk of prostate cancer and autoimmune disease. And women with tubal ligations have a higher chance of dangerous ectopic pregnancies.
Any Form of Emergency Contraception
Copper IUDs are sometimes used as emergency contraception. Emergency contraception, whether it’s a Plan B pill or a copper IUD has abortion-inducing properties. While it is a non-hormonal birth control option, I don’t recommend copper IUDs as emergency birth control.
Why I Don’t Recommend Herbs For Non-Hormonal Birth Control
Some herbs can work as contraceptives, but I will not list them or recommend them for several reasons:
- Many have abortifacient properties that can lead to early miscarriage.
- Most also impact the body in the same way that hormonal contraceptives do. So, they can cause similar problems for the mother as well. Herbs are effective and potent, and should be used with care. It’s important to avoid certain herbs for these reasons.
- None of the “contraceptive” herbs are 100% effective. They have side effects, and many can cause birth defects if conception does occur.
Natural Ways to Prevent or Delay Pregnancy
Artificial hormones aren’t something I want to take. But what if balancing hormones isn’t the reason for taking hormonal contraceptives? Maybe you truly need to delay or prevent pregnancy. In that case, there are better birth control options.
The following methods of contraception are much better for your body.
Non-Hormonal Birth Control: Natural Family Planning (NFP)
Natural Family Planning (NFP) or Fertility Awareness Methods (FAM) are natural methods of pregnancy prevention. But they can also help you get pregnant. They do this by focusing on natural hormonal cues.
These methods carry no side effects and help women get to know their bodies better. Some women discover problems (endometriosis, anovulation, etc.) from practicing these methods. A side benefit is that they help women be more in touch with their natural hormonal cues.
While these methods get a bad rap, they have come a long way from the Rhythm Methods of the past. Many are now as effective as hormonal methods (and more effective than barrier methods) when used consistently. It’s non-hormonal birth control that can either delay or achieve pregnancy. So if you decide to get pregnant, you don’t have to worry about infertility, birth defects, or delayed fertility after discontinuing.
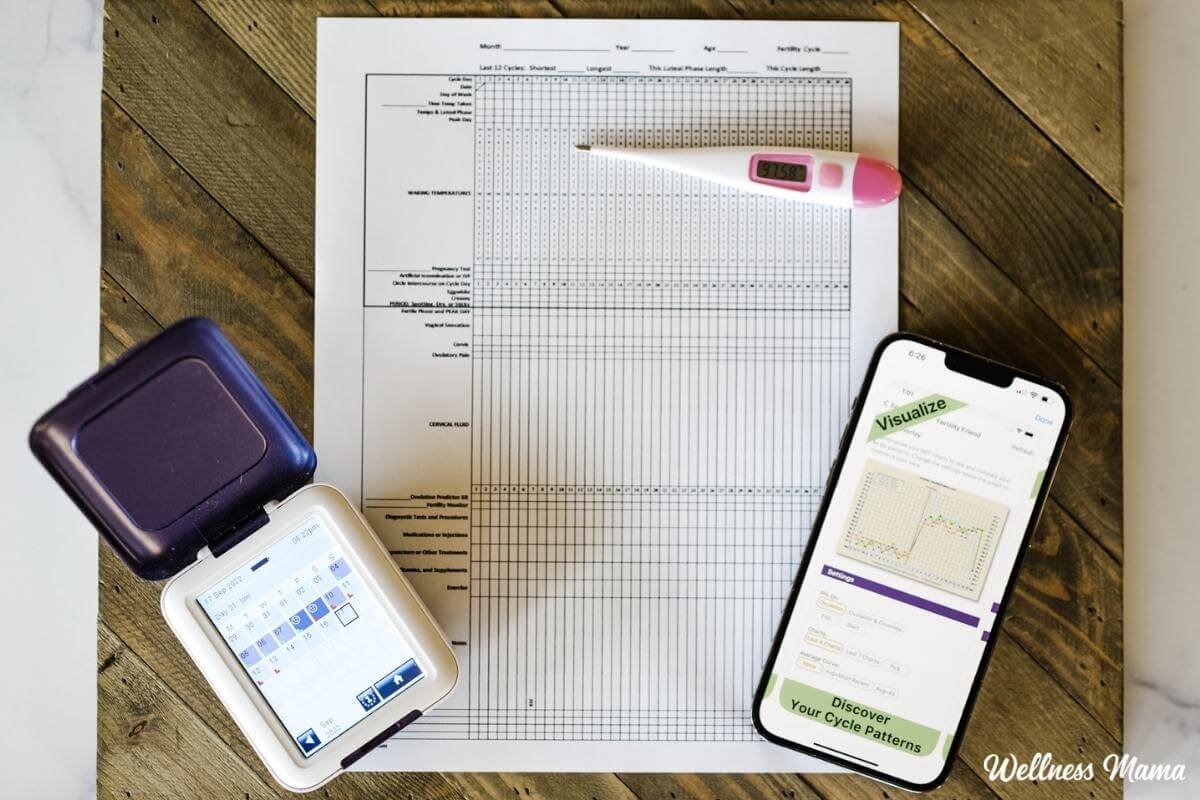
The basic concept is to use cues to predict ovulation and avoid sex when you’re fertile. These are things like basal body temperature (using a basal or BBT thermometer), mucus production, and cervical position. You can also use an ovulation calculator to find the fertile window in your menstrual cycle.
There are classes teaching how to practice these methods across the country. But for those who can’t find a class, there are websites like Fertility Friend. This free website allows users to chart their symptoms and pinpoint ovulation. There are even apps and mobile features for easy tracking.
High Tech NFP
After one of my pregnancies, I decided to go high-tech. I used a computer to do the NFP tracking and calculation for me. Thanks to emerging technology, there are several excellent options available now (I might use all listed):
- The Kegg fertility monitor relies on electrolyte level changes in cervical mucus so it’s more accurate than basal body thermometers alone. You can use their free app to look at your daily readings, trends, and fertility predictions. It only connects with the app via Bluetooth once it’s outside of your body, so there’s no EMF exposure.
- You can do NFP without a computer. All you need is a simple Basal Thermometer. Then you follow the method manually.
- Methods like ClearBlue monitors measure Luteinizing Hormones and estrogen to pinpoint ovulation. Though cheaper upfront, these require buying more ovulation strips, which you use daily. So, they can be more expensive in the long run.
- Fertile Focus – This is a simple and inexpensive fertility detector. The basic idea is that this microscope shows changes in saliva before ovulation. By examining saliva each day, you can predict when ovulation occurs.
Check out my complete reviews of these different fertility monitors here.
Good Old Fashioned Condoms
Male condoms are still the most popular form of non-hormonal birth control around the world. People like condoms because they’re both simple and effective and available over the counter. But they need a proper fit. To ensure a good fit, have your partner go to myONE Perfect Fit to find one that fits well. They have ten lengths, nine sizes, and 60 total options.
While condoms are a popular option based on medical information, they may not be a good option based on your faith or religious beliefs.
Caya Diaphragm for Non-Hormonal Birth Control
Using a diaphragm is another type of hormone-free birth control to look into. It’s a reusable cup that fits inside the vagina and over the cervix. The idea is to create a barrier between the uterus and sperm.
Most diaphragms are latex, which some people have allergies to. The Caya Contoured Diaphragm is silicone. Because it’s one-size-fits-all, it doesn’t need to be fitted by your doctor. You can buy it directly online or get a prescription from your pharmacist. It’s eco-friendly and gives you the option of occasional protection. It just requires a water-based spermicide. There are natural versions like lemon juice and others.
Be aware that because diaphragms can put pressure on your urethra, they are linked to urinary tract infections (UTIs).
Cervical Cap
A cervical cap is similar to a diaphragm in that it fits inside the vagina and over the cervix. The one available in the United States is called FemCap® and is made of silicon. For the best performance, it should be combined with a spermicide of some kind. Again, you can use a more natural version of this non-hormonal birth control.
Withdrawal or “Pull-Out” Option
If you prefer unprotected sex, you can have your man pull out his penis before ejaculation. You have to make sure to do it correctly every time. That is likely why it has a 22% failure rate. This form of non-hormonal birth control is popular but risky. You can make it more effective by combining it with a male condom.
What do you think? Ever used natural methods for balancing hormones or delaying pregnancy? Have other suggestions? Share below!

Leave a Reply