While I like the good kind of bugs in my GI tract, ticks are one bug I try hard to avoid. Each summer, when the leaves come out and the grass grows tall, many of us worry about tick-borne illness. As Lyme disease continues to rise, it’s crucial to explore natural ways to complement conventional treatments.
The best thing we can do is to support the body’s innate ability to heal.
What is Lyme Disease?
According to the Centers for Disease Control and Prevention (CDC), Lyme disease is a vector-borne disease. It’s most often spread through a tick bite, but it can also come through other biting insects like mosquitoes, spiders, and deer flies.
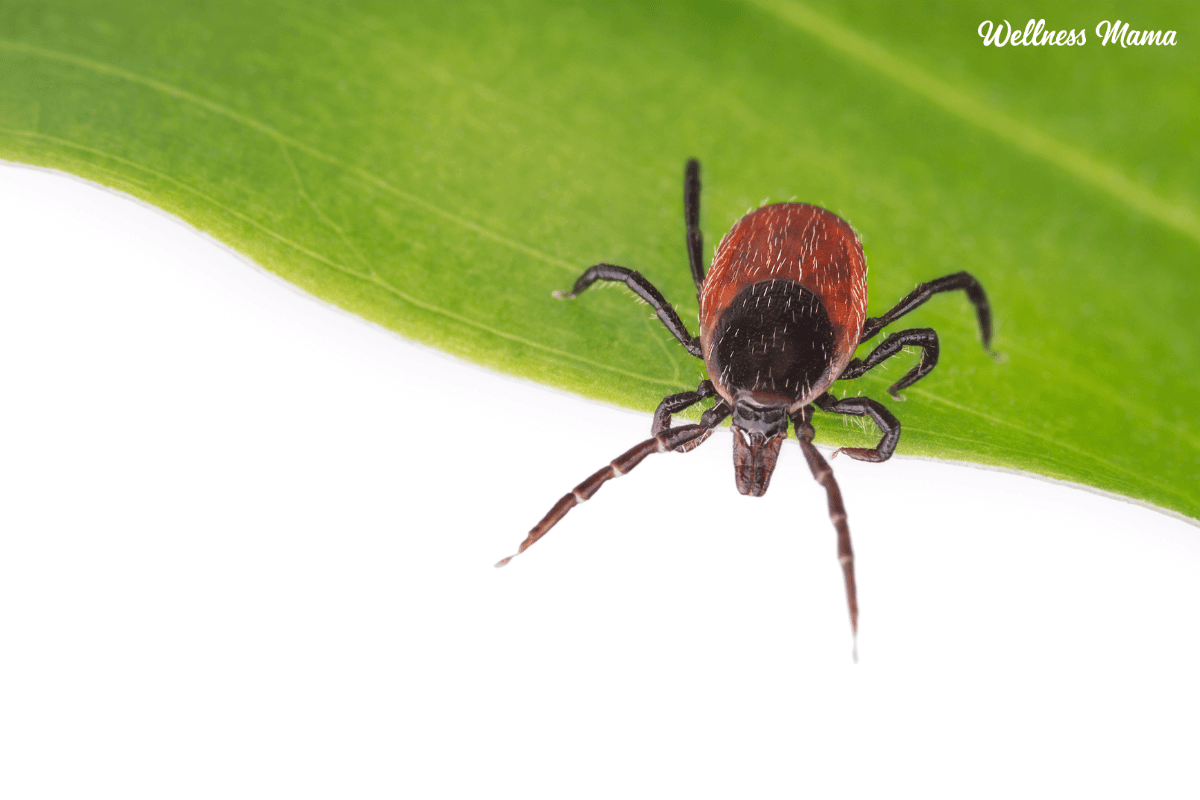
Lyme disease is caused by an infection of borrelia bacteria primarily carried by ticks. That’s why it’s also known as Lyme borreliosis. Lyme is most often caused by Borrelia burgdorferi but there are several different species depending on your area. Deer ticks (ixodes scapularis) or “blacklegged ticks” are the most common carriers in North America.
The first diagnosed case of Lyme disease was in Lyme, Connecticut, in the early 1970s; hence, the name. Originally, it was mistaken for an epidemic of juvenile rheumatoid arthritis due to its symptoms of joint pain and swelling, inflammation, and sometimes a fever and rash. Finally, the cause was identified as an infection in 1975.
How Do You Get Lyme?
A tick has three stages in its life cycle: larva, nymph, and adult. It’s during the nymph stage that ticks most often transmit Lyme disease. Nymph ticks are about the size of a poppy seed, so they’re easy to miss. They may stay attached for a few days before being discovered. They’re most active between the months of April and September – late spring to early fall.
Lyme disease is most common in the Northeast, mid-Atlantic states, and the Midwest. In states where Lyme disease is common, the incidence is currently about 40 cases per 100,000 individuals. However, it’s likely that Lyme is underdiagnosed.
The most tell-tale sign of Lyme disease is the bull’s-eye rash (erythema migrans). This may surround the site of the tick bite. However, most people never develop the bullseye rash, so it’s best to go in for testing. According to Johns Hopkins, many cases of Lyme are misdiagnosed as other diseases.
How Do You Test For Lyme Disease?
Testing for Lyme disease involves specific blood tests ordered by healthcare providers. These usually make up a two pro-pronged approach. The first test run is an antibody test like the ELISA screening. The ELISA is followed up by a second ELISA or an immunoblot test to confirm the results. That said, research shows the ELISA may be highly inaccurate and may miss about half of Lyme cases.
Later in the disease process, doctors may also order tests to look at the effects on the heart or brain.
One of the most reliable Lyme disease tests is through a company called Igenix., out of California. They not only test for Lyme but other tick-borne diseases as well. Examples include ehrlichiosis, which attacks the white blood cells, and babesiosis, which attacks the red blood cells. Others include anaplasmosis, spotted fever rickettsiosis, Rocky Mountain spotted fever, and Colorado tick fever. These co-infections can cause symptoms similar to Lyme disease.
Another more affordable option is Vibrant Wellness. The accuracy is comparable to Igenix but for less cost. You can get a full Lyme panel to test for different borrelia species as well as co-infections (which are common with Lyme).
If Lyme is left untreated, the infection may spread to the joints, heart, and nervous system. In the nervous system, it can even lead to meningitis or Bell’s palsy. Meningitis is inflammation of the membranes that cover the brain and spinal cord. Bell’s palsy causes facial weakness — usually on one side of the face. At that point, it has become chronic Lyme disease.
Chronic Lyme Disease
Mainstream scientists and doctors no longer acknowledge chronic Lyme disease as a legitimate condition. Instead, it’s being called post-treatment Lyme disease syndrome (PTLDS). They believe long-term symptoms only occur after treatment with antibiotics.
If there are chronic symptoms without antibiotic treatment, mainstream medicine won’t consider a Lyme infection. Instead, they’ll point to chronic fatigue syndrome or fibromyalgia, which they’ll admit may be caused by an infection. Some experts even claim those who talk about chronic Lyme disease are committing health fraud.
Symptoms of Lyme Disease
There are three stages of Lyme disease: 1) early localized, 2) early disseminated, and 3) late disseminated. In the early stages, Lyme disease can cause the bull’s-eye rash and flu-like symptoms. These show up anywhere from three days to 30 days after the tick bite. Early signs and symptoms of Lyme disease may include:
- Flu-like symptoms, such as fever and chills
- Headache
- Fatigue
- Muscle pain and joint pain
- Swollen lymph nodes
- Erythema migrans (bull’s-eye, red, or blue/red) rash
Later signs and symptoms of Lyme disease may include:
- Severe headaches and neck stiffness
- Additional Erythema migrans rashes in other parts of the body
- Arthritis in large joints like the knees or hips
- Facial palsy
- Pain that comes and goes in muscles, joints, tendons, and bones
- Lyme arthritis
- Irregular heartbeat (Lyme carditis)
- Neurological symptoms, including nerve pain, numbness, and tingling in the hands or feet
These late disseminated symptoms may occur if Lyme is left untreated, disrupting multiple systems. Some people don’t receive a Lyme diagnosis until after they’ve been through years or even decades of debilitating symptoms.
How Does a Clinic Treat Lyme?
Tick removal is the first step. Use tweezers, a “tick tornado,” or another tick removal tool to safely remove the tick, still intact. Prompt removal of ticks can reduce the likelihood of infection. I keep a tick remover on my keychain during tick season. Here are more details on how to remove a tick (the right way!).
The mainstream medical treatment for Lyme disease is to give an antibiotic soon after a bite by an infected tick. The antibiotics generally used for Lyme are doxycycline, amoxicillin, azithromycin, and cefuroxime. These antibiotics may be given in intravenous (IV) form if the condition is severe enough.
Patients are typically given a 2 week course of oral antibiotics. However in order to be effective Lyme literate medical doctors (LLMD) recommend a minimum of 6 weeks of doxycycline.
Scientists are also working tirelessly to create a Lyme disease vaccine designed to address an “important public health problem.” That’s a discussion for another time.
To avoid getting bitten again, mainstream clinicians usually recommend finding a bug spray with DEET. But DEET has problems of its own as a known neurotoxin. You can also treat clothing before going out into high tick areas with permethrin. But again, it has risks if it gets on the skin or you breathe it.
How Do You Treat Lyme Disease Naturally?
It’s possible to address Lyme naturally. Some people even opt for natural remedies alongside or following antibiotics. Some of the strategies for helping the immune system eliminate Lyme and coinfections include the following:
- Certain herbs have shown promise for Lyme disease: Examples include cat’s claw, Japanese knotweed, andrographis, wormwood, black walnut, Chinese skullcap, and Cistus incanus. There are several more that may be combined in a blend.
- Homeopathic remedy: Ledum Palustre is a homeopathic medicine for insect bites and may be helpful for Lyme-related infections. Practitioners recommend taking this as soon as you remove the tick to help prevent an infection from developing.
- Hyperbaric Oxygen Therapy (HBOT): Hyperbaric therapy may be helpful for killing infections that don’t like high oxygen environments. Lyme is one of those infections.
- Ozone therapy: Ozone in its various forms may be helpful for the same reason as HBOT — increasing oxygen throughout the tissues to fight infections.
- Bee venom therapy: Bee venom is naturally antimicrobial. Scientists have done studies on whole bee venom or a key component, melittin, for Lyme disease. Both the whole venom and melittin showed promise for fighting Lyme bacteria.
- Ivermectin: Ivermectin isn’t considered a primary treatment for Lyme disease. However, some people report improvement when taking the anti-parasite medication ivermectin daily over several months. Parasitic infections can hamper Lyme treatment so it’s important to treat these too.
- Essential oils: Oregano, clove, and cinnamon oil have antimicrobial properties shown to be effective against Lyme bacteria in studies by Johns Hopkins.
Other treatments include:
- Intravenous nutrients
- General immune support
- Detoxification support
- Mast cell and histamine support
- Anti-virals
- Anti-parasitics
- And general support of the body.
The immune system is designed to fight all infections. When stress, toxins, and other infections overburden our body we’re more susceptible to chronic infections like viruses, parasites, and Lyme disease.
Enlist Help
Lyme disease treatment can get complicated and there are almost always other coinfections and factors involved. It can be really helpful to find a Lyme practitioner to help you through the process. Finding a good one can be tough though. Some people rely on doing their own research and ordering testing as needed. You can do this online or sometimes through your regular doctor.
Here are a few resources to help:
- Homeopathic protocol for Lyme
- 102: Dr. Jay Davidson on Staying Safe From Ticks & Avoiding Chronic Lyme Disease
- 173: Dr. Jaban Moore on the Inflammation Model of Chronic Disease (including Lyme)
- Toxic: Heal Your Body from Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Chronic Environmental Illness by Neil Nathan, M.D.
- Healing Lyme: Natural Healing of Lyme Borreliosis and the Coinfections Chlamydia and Spotted Fever Rickettsiosis by Stephen Buhner and Dr. Neil Nathan
- Healing Lyme Disease Coinfections by Stephen Buhner
Take Precautions and Prevent Lyme Disease!
The best way to prevent Lyme disease is to avoid being bitten in the first place. Here are some things you can do to lessen your chances of having a tick crawling around and attaching:
- Wear long pants when heading to wooded areas.
- Opt for light-colored clothing with a long-sleeved shirt
- Use a natural insect repellent with essential oils.
- Avoid walking in tall grasses or near shrubs.
- Tuck your pants into your socks.
- Wear a hat or put hair up.
- Remove clothing immediately after returning home.
- Do a full body check using a mirror, and then take a shower.
- Check common areas where ticks attach, such as under the arms, in or around the hair, in or around the ears, around the waist, the back of the knees, between the legs, or even inside the belly button.
These are excellent practices when spending time outdoors. But you can also make yourself more resistant to infections and more resilient when exposed.
Final Thoughts on Ticks and Lyme
Like all infectious diseases, Lyme is more likely to occur in those of us whose immune systems are worn down. Taking care of yourself by eating properly, getting enough sleep, and reducing stress can make you a less-appealing victim.
The source of Lyme disease and response to treatment can vary widely. Some people may recover fully with timely and appropriate treatment. But others may experience persistent symptoms that require ongoing care. Each experience with Lyme is unique, and personalized care is essential.
Have you successfully overcome Lyme disease? What worked for you? Share with us below!


Leave a Reply